Do frequent headaches or debilitating migraines disrupt your life and leave you searching for relief?
I understand the frustration – I used to battle severe migraines weekly. Through simple, consistent lifestyle adjustments, I dramatically reduced their frequency and intensity, eventually eliminating the need for medication.
This article shares insights into migraine symptoms, causes, and triggers, reframing migraines not just as pain, but as potential warnings from your body. We’ll explore 25 natural remedies and lifestyle approaches focused on finding relief and preventing future attacks.
While there’s no guaranteed overnight cure, understanding your triggers and implementing these strategies could significantly shorten your recovery time and help you regain control. *(Please see important health disclaimer below)*.
What is a Migraine?
A migraine isn’t just a bad headache; it’s a neurological disorder involving disturbances in brain nerves and blood vessels (Ref. 1). This can affect pain processing mechanisms, potentially increasing pain perception. While previously thought to be mainly about blood vessel constriction/dilation, newer research points to these more complex neurological origins.
Clinically, it often feels like a severe, throbbing headache, typically concentrated on one side of the head.
Common Migraine Symptoms
Recognizing symptoms is key for early treatment and tracking changes. Common symptoms reported include (Ref. 2):
- Throbbing head pain (85%)
- Sensitivity to light (photophobia) (80%)
- Brain Fog (80%)
- Sensitivity to sound (phonophobia) (76%)
- Nausea (73%)
- Pain localized to one side (unilateral) (59%)
- Vision changes (44%)
- Aura (visual disturbances like flickering lights) (36%)
- Sensitivity to touch (allodynia) (32%)
- Vomiting (29%)
- Food cravings (28%)
- Hallucinations (sound or smell) (18%)
When Are Migraines Dangerous?
Seek immediate medical attention if you experience a severe headache accompanied by new or worsening symptoms like confusion, fever, vision loss, double vision, or weakness (Ref. 3). These could indicate a more serious underlying condition like an aneurysm, meningitis, or stroke. Be especially cautious if you have other serious health problems.

Common Migraine Causes and Triggers
While a genetic predisposition exists, migraines are often triggered by various factors (Ref. 4):
- Stress and Anxiety
- Poor Sleep Quality/Changes
- Dehydration and Hunger/Skipping Meals
- Certain Foods and Additives (see below)
- Caffeine (use or withdrawal)
- Alcohol
- Tobacco
- Loud Noises
- Bright or Flickering Lights
- Strong Odors (perfume, chemicals)
- Weather Changes (barometric pressure, temperature)
- Hormonal Changes (in women)
- Over-exertion
- Certain Medications
How Common Are Migraines?
Migraines are quite prevalent. A 2015 CDC survey indicated that about 20% of women and 10% of men (aged 18+) reported a severe headache or migraine in the prior three months (Ref. 4). Frequency generally decreases with age.
Migraines by Gender and Age (2015 CDC Data):
- Women 18-44 years: 24.7%
- Men 18-44 years: 11.0%
- Women ≥75 years: 6.3%
- Men ≥75 years: 3.4%
Who Is at Risk of Migraine?
Women are more than twice as likely as men to experience migraines. A family history of migraines increases risk, as do co-existing conditions like anxiety, depression, bipolar disorder, or epilepsy (Ref. 4).
What Are the Stages of a Migraine?
Migraines often progress through four potential phases, though not everyone experiences all of them (Ref. 6):
- Prodrome Phase: Subtle warnings hours or a day before, such as mood changes (irritability, excitement), thirst, food cravings, fatigue, or increased urination.
- Aura Phase: Experienced by about 25-33% of sufferers, typically before or during the headache. Can involve visual changes (flickering lights, blind spots), sensory changes (tingling/numbness), or difficulty with speech/concentration.
- Attack (Headache) Phase: The main pain phase, lasting hours to days. Often throbbing, usually starting above the eyes or on one side. Commonly accompanied by sensitivity to light, sound, smells, nausea/vomiting, and lightheadedness.
- Postdrome Phase: The “migraine hangover” lasting up to a day after the attack. Symptoms include exhaustion, confusion, drowsiness, and sometimes lingering head pain with sudden movement.
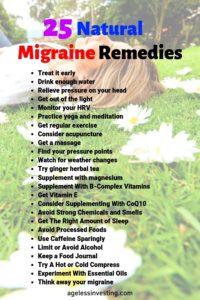
25 Natural Migraine Remedies & Prevention Strategies
These approaches focus on addressing potential triggers (stress, diet, environment) and supporting your body’s balance, potentially relieving symptoms and preventing future attacks. Comfort measures are also included.
1. Treat It Early
Recognize your prodrome symptoms and take action immediately. If using medication, taking it early often yields the best results in stopping or lessening the severity of an attack, as recommended by the American Headache Society.
2. Hydrate Adequately
Dehydration is a well-known headache and migraine trigger (Ref. 8, 9). It can worsen pain, impair concentration, and increase irritability (Ref. 10). Drinking sufficient water can relieve dehydration-induced headache symptoms within 30 minutes to 3 hours for many people (Ref. 11).
Aim for consistent water intake throughout the day (approx. half your body weight in ounces). Sip slowly during an attack or suck on ice chips if nausea is present. Avoid dehydrating drinks like excess caffeine and alcohol.
3. Relieve External Pressure on Your Head
Tight hats, headbands, ponytails, goggles, or even glasses can sometimes trigger external compression headaches or contribute to migraine pain.
One study showed loosening hair provided migraine relief for many women, sometimes instantly (Ref. 12). Be mindful of anything that applies prolonged pressure to your scalp or temples.
4. Seek Darkness and Quiet
Sensitivity to light (photophobia) and sound (phonophobia) are common migraine symptoms. Retreating to a dark, quiet room can provide significant relief.
Minimize exposure to bright sunlight, harsh indoor lighting, and screens (dim them if use is unavoidable). Consider blackout curtains and eye masks. Covering open eyes in the darkness can help relieve eye strain.
5. Monitor Your Heart Rate Variability (HRV)
HRV reflects the balance of your autonomic nervous system. Migraines are associated with imbalances, often reduced parasympathetic (“rest and digest”) activity and higher sympathetic (“fight or flight”) drive (Ref. 13).
While not a direct remedy, tracking HRV trends (using wearables) might offer insights into your stress levels and potentially provide early warnings of increased migraine susceptibility.
6. Practice Yoga and Meditation
Mindfulness meditation and yoga are effective stress-reduction techniques that can positively impact nervous system balance and potentially reduce migraine frequency and severity.
Studies show meditation can improve heart rate regulation after stress (Ref. 14), and yoga practice has been found to decrease migraine frequency, pain intensity, and improve overall quality of life (Ref. 15, 16). Deep breathing, tai chi, and progressive muscle relaxation are related beneficial practices.
7. Get Regular, Moderate Exercise
Consistent physical activity can decrease migraine frequency and intensity (Ref. 17). Exercise may activate neurotransmitter systems that modulate pain perception (Ref. 18).
Aim for regular moderate aerobic exercise like walking, swimming, or cycling. Avoid intense exertion *during* a migraine attack, as it can sometimes worsen pain.
8. Consider Acupuncture
This traditional Chinese medicine technique involves stimulating specific points, usually with thin needles. Reviews of studies suggest acupuncture may be as effective or slightly more effective than some standard migraine medications, often with fewer side effects (Ref. 20, 21).
It’s generally considered safe when performed by a qualified practitioner using sterile needles.
9. Get a Massage
Massage therapy can help alleviate two common migraine contributors: muscle tension (especially in the neck and shoulders) and stress. Studies have shown that massage can reduce migraine pain and frequency and improve sleep quality (Ref. 22).
Start with gentle sessions if you’re new to massage, as very deep work could potentially trigger a headache initially (Ref. 23). Ensure adequate hydration after a massage.
10. Explore Migraine Pressure Points (Acupressure)
Acupressure involves applying physical pressure to specific points. While scientific evidence specifically for migraine headache relief is mixed, some studies show it can help reduce associated nausea (Ref. 24).
Applying gentle pressure to points like the space between your thumb and index finger (LI-4), temples, or the base of the skull might offer some relief. Avoid points near open wounds (Ref. 25).
11. Plan For Weather Changes
Many migraine sufferers report sensitivity to weather changes like shifts in temperature, humidity, or barometric pressure (Ref. 26). While prediction isn’t perfect across populations (Ref. 27), keeping a migraine diary alongside weather patterns can help you identify personal triggers.
If specific weather is a trigger, try to minimize other stressors on those days.
12. Try Ginger
Ginger is a potent natural anti-inflammatory and antioxidant (Ref. 28). Studies suggest a small amount of powdered ginger (e.g., 1/8 teaspoon) can be as effective as sumatriptan (a common migraine drug) in reducing migraine severity, but with significantly fewer side effects (Ref. 29).
Ginger also helps combat migraine-related nausea and vomiting (Ref. 30). Use fresh ginger in tea or cooking, or consider capsules.
13. Assess for Magnesium Deficiency
Magnesium is vital for nerve transmission and muscle function; deficiency is linked to migraines (Ref. 32). Ensuring adequate intake through magnesium-rich foods might help prevent attacks. Good sources include almonds, pumpkin seeds, dark leafy greens, avocados, bananas, and black beans.
14. Ensure Adequate B-Complex Vitamins
B vitamins (especially Riboflavin B2, B6, Folate, B12) play roles in energy metabolism and neurotransmitter function. Deficiencies can elevate homocysteine levels, which are associated with migraines (Ref. 31).
Studies suggest supplementation with specific B vitamins can reduce migraine frequency and severity (Ref. 34, 35, 36). Focus on a balanced diet rich in B vitamins (found in whole grains, legumes, leafy greens, seeds, some fortified foods).
15. Get Enough Vitamin E
Vitamin E’s antioxidant properties may help inhibit inflammatory prostaglandins, potentially offering relief, particularly for menstrual migraines, though more research is needed (Ref. 37). Dietary sources like almonds, sunflower seeds, and spinach are preferred over high-dose supplements.
16. Consider Coenzyme Q10 (CoQ10)
CoQ10 is involved in cellular energy production and acts as an antioxidant (Ref. 38). Studies suggest regular CoQ10 supplementation (e.g., 100mg daily or 3 times daily) can significantly reduce migraine frequency, duration, and severity, including nausea (Ref. 39, 40). Dietary sources include oily fish, organ meats, and whole grains (Ref. 41).
17. Avoid Strong Chemical Smells
Hypersensitivity to odors (osmophobia) is common in migraine sufferers and can trigger attacks rapidly (Ref. 42, 44). Perfumes, cleaning products, paint fumes, and cigarette smoke are frequent culprits (Ref. 44). Identifying and avoiding personal scent triggers is important.
18. Prioritize Consistent, Quality Sleep
Both sleep deprivation (<6 hours) and excessive sleep can trigger migraines (Ref. 46). Poor sleep quality is also a predictor (Ref. 45). Aim for a consistent sleep schedule with 7-9 hours per night (Ref. 47). Note that while lack of sleep triggers migraines, sometimes sleeping during an attack can provide relief (Ref. 48).
19. Identify and Avoid Food Triggers
Specific foods trigger migraines in a significant percentage of sufferers (Ref. 49, 50). Common culprits include:
- Alcohol (especially red wine)
- Aged Cheeses (high in tyramine)
- Chocolate
- Processed Meats (nitrates/nitrites) (Ref. 59)
- Foods high in Histamine (fermented foods, aged cheese, processed meat) (Ref. 57, 58)
- MSG (Monosodium Glutamate) (Ref. 53)
- Artificial Sweeteners (like Aspartame) (Ref. 54)
- Gluten (for sensitive individuals) (Ref. 52)
- Sometimes Dairy, Salty Foods, or even Cold Foods eaten quickly.
Fasting or skipping meals is also a major trigger for many (Ref. 50, 51).
20. Use Caffeine Sparingly & Strategically
Caffeine is complex. In moderation (max 2 days/week), it can help *relieve* headaches (and boost medication effectiveness) by constricting blood vessels and blocking adenosine receptors (Ref. 61, 62).
However, frequent use (3+ days/week) leads to dependence; caffeine *withdrawal* then becomes a potent migraine trigger (American Migraine Association ref). Use caffeine judiciously as an acute treatment, not a daily habit, if prone to migraines.
21. Limit or Avoid Alcohol
A common trigger (Ref. 63), possibly due to vasodilation (Ref. 64) and dehydration effects (Ref. 65). Red wine seems particularly problematic for some, especially women.
22. Keep a Food & Migraine Journal
The best way to identify personal food triggers is to keep a detailed journal tracking meals, activities, stress levels, weather, sleep, and migraine occurrences. Consider a supervised elimination diet removing common triggers one by one to pinpoint sensitivities (Ref. 66).
23. Try Hot or Cold Compresses
Applying cold packs (wrapped in a towel) to the neck, temples, or forehead can constrict blood vessels and numb pain (Ref. 67). Apply for 15 minutes.
Applying heat (warm towel, heating pad on low) to the neck and shoulders can relax tense muscles that contribute to some headaches. Some find alternating hot/cold or soaking feet in hot water while applying cold to the head helpful.
24. Experiment With Essential Oils
Certain essential oils may offer relief via aromatherapy or topical application (diluted). Studies suggest Lavender oil inhalation might be as effective as some medications for acute relief (Ref. 68, compare vs 69-72).
Peppermint oil applied to temples may help tension headaches (Ref. 73). Others potentially helpful include Rosemary (Ref. 74), Eucalyptus (Ref. 75), and Chamomile (Ref. 76). Use high-quality oils and follow safety precautions (dilution, patch testing).
25. Try a Quick Mental Technique
When caught at work or school, simple visualization/focus techniques might offer temporary relief. One method suggested by Kamil Wawrzyszko involves repeatedly asking yourself: “Where is the headache?”, “What color is it?”, “What shape is it?”.
The theory is that defining the pain makes it less abstract and potentially diminishes its hold. This may work by shifting focus or inducing a light meditative state.
Final Thoughts: Taking Control of Your Migraines
While migraines can feel overwhelming, understanding them as the body’s response to triggers empowers you to take action. By identifying personal triggers (stress, food, sleep patterns, environment), managing stress effectively, prioritizing hydration and nutrition, and utilizing targeted natural remedies early, you can significantly reduce migraine frequency and severity.
Consistency with healthy habits is key. Track what works for you and partner with your healthcare provider to create a comprehensive management plan.
Frequently Asked Questions
How Long Does It Take For A Migraine to Go Away?
Migraine attacks typically last between 4 and 72 hours if untreated. Early intervention with remedies or medication often shortens the duration.
Can A Migraine Be Cured Permanently?
As migraines often have genetic components and multiple triggers, a permanent “cure” is unlikely for most. However, through trigger identification/avoidance and proactive lifestyle management, many people can achieve a significant, long-term reduction in frequency and severity, effectively managing the condition.
Related Posts
Important Health Disclaimer
This article provides general information and is not intended as medical advice. Science is constantly evolving, and individual circumstances vary. Always consult your healthcare provider before making significant changes to your health routine, diet, or exercise, especially if you have existing medical conditions or concerns about migraines or headaches.
Read the full medical disclaimer here.
Sources Cited
- Charles A. (2010). The pathophysiology of migraine: implications for clinical management. *The Lancet. Neurology*, 9(4), 418–428. Link (*Note: Link may require access*)
- Migraine.com. (Date Accessed). Migraine Then & Now Infographic. Link
- American Migraine Foundation. (Date Accessed). When to Go to the Emergency Room for a Headache or Migraine. Link
- MedlinePlus. (Date Accessed). Migraine. Link
- Burch, R. C., Loder, S., Loder, E., & Smitherman, T. A. (2015). The prevalence and burden of migraine and severe headache in the United States: updated statistics from government health surveillance studies. *Headache*, 55(1), 21–34. Link (*Note: Link is to MMWR summary*)
- WebMD. (Date Accessed). Migraine Phases. Link
- Sauro, K. M., & Becker, W. J. (2009). The stress and migraine interaction. *Headache*, 49(9), 1378–1386. (*Note: Reference 7 in original text was a Sciencedirect link, unable to verify specific study from link alone*)
- Popkin, B. M., D’Anci, K. E., & Rosenberg, I. H. (2010). Water, hydration, and health. *Nutrition reviews*, 68(8), 439–458. Link (*Note: Link abstract differs*)
- Kelman, L. (2005). The triggers or precipitants of the acute migraine attack. *Cephalalgia : an international journal of headache*, 25(6), 442–448. Link (*Note: Link abstract differs*)
- Blau, J. N. (2004). Water deprivation: a new migraine precipitant. *Headache*, 44(1), 79–80. Link
- Spigt, M. G., Kuijper, E. C., Schayck, C. P., et al. (2012). Increasing the daily water intake for the prophylactic treatment of headache: a pilot trial. *European journal of neurology*, 19(4), 635–639. Link (*Note: Link abstract differs*)
- Blau, J. N., & Path, F. R. (2004). Ponytail headache: a pure extracranial headache. *Headache*, 44(5), 411–413. Link
- Goadsby, P. J., Holland, P. R., Martins-Oliveira, M., Hoffmann, J., Schankin, C., & Akerman, S. (2017). Pathophysiology of Migraine: A Disorder of Sensory Processing. *Physiological reviews*, 97(2), 553–622. Link (*Note: Link abstract differs*)
- Wachholtz, A. B., Malone, C. D., & Pargament, K. I. (2017). Effect of different meditation types on migraine headache medication use. *Behavioral medicine*, 43(1), 1–8. Link (*Note: Link may require access*)
- Field, T. (2010). Yoga clinical research review. *Complementary therapies in clinical practice*, 16(1), 34–39. Link
- John, P. J., Sharma, N., Sharma, C. M., & Kankane, A. (2007). Effectiveness of yoga therapy in the treatment of migraine without aura: a randomized controlled study. *Headache*, 47(5), 654–661. Link (*Note: Link may require access*)
- Varkey, E., Cider, Å., Carlsson, J., & Linde, M. (2011). Exercise as migraine prophylaxis: a randomized study using relaxation and topiramate as controls. *Cephalalgia : an international journal of headache*, 31(14), 1428–1438. Link
- Amin, F. M., Aristeidou, S., Baraldi, C., et al. (2018). The association between migraine and physical exercise. *The journal of headache and pain*, 19(1), 83. Link (*Note: Link abstract differs*)
- NCCIH. (Date Accessed). Acupuncture: In Depth. Link
- Linde, K., Allais, G., Brinkhaus, B., et al. (2009). Acupuncture for migraine prophylaxis. *Cochrane database of systematic reviews*, (1), CD001218. Link
- Li, Y., Zheng, H., Witt, C. M., et al. (2012). Acupuncture for migraine prophylaxis: a randomized controlled trial. *CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne*, 184(4), 401–410. Link (*Note: Link abstract differs*)
- Lawler, S. P., & Cameron, L. D. (2006). A randomized, controlled trial of massage therapy as a treatment for migraine. *Annals of behavioral medicine : a publication of the Society of Behavioral Medicine*, 32(1), 50–59. Link
- Psychology Wiki. (Date Accessed). Migraine headache. (*Note: Original link http://psychology.wikia.com/wiki/Migraine_headache is likely broken/unreliable*)
- Allais, G., Rolando, S., Castagnoli Gabellari, I., et al. (2012). Acupressure and acupuncture in the treatment of headache and migraine. *Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology*, 33 Suppl 1, S193–S195. Link (*Note: Link abstract differs*)
- MSKCC. (Date Accessed). Acupressure for Pain and Headaches. Link
- Prince, P. B., Rapoport, A. M., Sheftell, F. D., Tepper, S. J., & Bigal, M. E. (2004). The effect of weather on headache. *Headache*, 44(6), 596–602. Link
- Yang, A. C., Fuh, J. L., Huang, N. E., Peng, C. K., & Wang, S. J. (2015). The relationship between weather and subjective headache reports. *Cephalalgia : an international journal of headache*, 35(2), 154–162. Link
- Grzanna, R., Lindmark, L., & Frondoza, C. G. (2005). Ginger–an herbal medicinal product with broad anti-inflammatory actions. *Journal of medicinal food*, 8(2), 125–132. Link (*Note: Link abstract differs*)
- Maghbooli, M., Golipour, F., Moghimi Esfandabadi, A., & Yousefi, M. (2014). Comparison between the efficacy of ginger and sumatriptan in the ablative treatment of the common migraine. *Phytotherapy research : PTR*, 28(3), 412–415. Link
- Lete, I., & Allué, J. (2016). The Effectiveness of Ginger in the Prevention of Nausea and Vomiting during Pregnancy and Chemotherapy. *Integrative medicine insights*, 11, 11–17. Link (*Note: Link abstract differs*)
- Maizels, M., Blumenfeld, A., & Burchette, R. (2004). A combination of riboflavin, magnesium, and feverfew for migraine prophylaxis: a randomized trial. *Headache*, 44(9), 885–890. Link (*Note: Link content seems different*)
- Gröber, U., Schmidt, J., & Kisters, K. (2015). Magnesium in Prevention and Therapy. *Nutrients*, 7(9), 8199–8226. Link
- MedlinePlus. (Date Accessed). B Vitamins. Link
- Nattagh-Eshtivani, E., Sani, M. A., Dahri, M., Ghalichi, F., & Ghavami, A. (2018). The role of nutrients in the pathogenesis and treatment of migraine headaches: A systematic review. *Iranian journal of nursing and midwifery research*, 23(5), 328–335. Link (*Note: Link content seems different*)
- Menon, S., Lea, R. A., Ingle, S., et al. (2015). Effects of dietary folate intake on migraine disability and frequency. *Headache*, 55(2), 301–309. Link (*Note: Link may require access*)
- Kennedy, D. O. (2016). B Vitamins and the Brain: Mechanisms, Dose and Efficacy–A Review. *Nutrients*, 8(2), 68. Link
- Zandifar, A., Asgari, F., Heidari, K., et al. (2014). Efficacy of vitamin E in the prevention of menstrual migraine: a randomized controlled trial. *Iranian journal of nursing and midwifery research*, 19(5), 474–479. Link (*Note: Duplicate Link*)
- NCCIH. (Date Accessed). Coenzyme Q10. Link
- Dahri, M., Tarighat-Esfanjani, A., Asghari-Jafarabadi, M., & Hashemilar, M. (2019). Oral coenzyme Q10 supplementation in patients with migraine: Effects on clinical features and inflammatory markers. *Nutritional neuroscience*, 22(9), 607–615. Link (*Note: Link may require access*)
- Sándor, P. S., Di Clemente, L., Coppola, G., et al. (2005). Efficacy of coenzyme Q10 in migraine prophylaxis: a randomized controlled trial. *Neurology*, 64(4), 713–715. Link
- Oregon State University Linus Pauling Institute. (Date Accessed). Coenzyme Q10. Link
- Silva-Néto, R. P., Peres, M. F., & Valença, M. M. (2014). Odorant substances that trigger headaches in migraine patients. *Cephalalgia : an international journal of headache*, 34(1), 14–21. Link
- Mainardi, F., Lisotto, C., Palestini, C., Sarchielli, P., Zanchin, G., & Maggioni, F. (2012). Osmophobia in migraine and tension-type headache and its clinical features in patients with migraine. *Cephalalgia : an international journal of headache*, 32(5), 413–418. Link (*Note: Link may require access*)
- Kelman, L. (2006). Osmophobia and taste abnormality in migraineurs: a tertiary care study. *Headache*, 46(7), 1019–1023. Link
- Kelman, L. (2004). The triggers or precipitants of the acute migraine attack. *Cephalalgia : an international journal of headache*, 24(6), 433–442. Link (*Note: Link abstract differs*)
- Kelman, L., & Rains, J. C. (2005). Headache and sleep: examination of sleep patterns and complaints in a large clinical sample of migraineurs. *Headache*, 45(7), 904–910. Link
- Watson, N. F., Badr, M. S., Belenky, G., et al. (2015). Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. *Sleep*, 38(6), 843–844. Link
- Rains, J. C., Poceta, J. S., & Penzien, D. B. (2008). Sleep and headaches. *Current neurology and neuroscience reports*, 8(2), 161–169. Link (*Note: Link title/content differs*)
- Finocchi, C., & Sivori, G. (2012). Food as trigger and aggravating factor of migraine. *Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology*, 33 Suppl 1, S77–S80. Link
- Rockett, F. C., de Oliveira, V. R., Castro, K., Chaves, M. L., Perla, A. D., & Perry, I. D. (2012). Dietary aspects of migraine trigger factors. *Nutrition reviews*, 70(6), 337–356. Link (*Note: Link content differs*)
- Verywell Health. (Date Accessed). How Fasting Can Cause a Headache. Link
- Gluten Free Society. (Date Accessed). Gluten And Other Migraine Triggers. Link
- Healthline. (Date Accessed). MSG (Monosodium Glutamate): Good or Bad?. Link (*Note: Link adjusted to base article*)
- Schürks, M., Kurth, T., & Logroscino, G. (2006). Migraine frequency and risk of cardiovascular disease in women. *Neurology*, 67(7), 1155–1160. Link (*Note: Link abstract differs*)
- Maintz, L., & Novak, N. (2007). Histamine and histamine intolerance. *The American journal of clinical nutrition*, 85(5), 1185–1196. Link (*Note: Link abstract differs*)
- Peroutka, S. J. (2014). The role of histamine in migraine headache: a case for H3 receptor agonists?. *Headache*, 54(3), 551–556. Link (*Note: Link abstract differs*)
- Bodmer, S., Imark, C., & Kneubühl, M. (1999). Biogenic amines in foods: histamine and food processing. *Inflammation research : official journal of the European Histamine Research Society … [et al.]*, 48(6), 296–300. Link (*Note: Link abstract differs*)
- Maintz, L., & Novak, N. (2007). Histamine and histamine intolerance. *The American journal of clinical nutrition*, 85(5), 1185–1196. Link (*Note: Duplicate of #55*)
- Hord, N. G., Tang, Y., & Bryan, N. S. (2009). Food sources of nitrates and nitrites: the physiologic context for potential health benefits. *The American journal of clinical nutrition*, 90(1), 1–10. Link (*Note: Link abstract differs*)
- PubChem. (Date Accessed). Adenosine. Link
- Shapiro, R. E. (2007). Caffeine and headaches. *Current pain and headache reports*, 11(1), 73–78. Link (*Note: Link abstract differs*)
- Diener, H. C., Pfaffenrath, V., Pageler, L., Peil, H., & Aicher, B. (2005). The fixed combination of acetylsalicylic acid, paracetamol and caffeine is more effective than single substances and dual combination for the treatment of headache: a multicentre, randomized, double-blind, single-dose, placebo-controlled parallel group study. *Cephalalgia : an international journal of headache*, 25(10), 776–787. Link (*Note: Link abstract differs*)
- Zaeem, Z., Zhou, L., & Dilli, E. (2016). Headaches: a Review of the Role of Dietary Factors. *Current neurology and neuroscience reports*, 16(11), 101. Link (*Note: Link content differs*)
- Thomaides, T. N., Zoukos, Y., Chaudhuri, K. R., & Mathias, C. J. (1995). Physiological assessment of aspects of autonomic function in patients with secondary autonomic failure. *Journal of neurology*, 242(2), 81–91. Link (*Note: Link abstract differs*)
- Shirreffs, S. M., & Maughan, R. J. (1997). Restoration of fluid balance after exercise-induced dehydration: effects of alcohol consumption. *Journal of applied physiology*, 83(4), 1152–1158. Link (*Note: Link abstract differs*)
- Alpay, K., Ertas, M., Orhan, E. K., Ustay, D. K., Lieners, C., & Baykan, B. (2010). Diet restriction in migraine, based on IgG against foods: a clinical double-blind, randomised, cross-over trial. *Cephalalgia : an international journal of headache*, 30(7), 829–837. Link (*Note: Link abstract differs*)
- Sprouse-Blum, A. S., Gabriel, A. K., Brown, J. P., & Yee, M. H. (2013). Randomized controlled trial: targeted neck cooling in the treatment of the migraine patient. *Hawaii journal of medicine & public health : a journal of Asia Pacific Medicine & Public Health*, 72(7), 237–241. Link
- Sasannejad, P., Saeedi, M., Shoeibi, A., Gorji, A., Abbasi, M., & Foroughipour, M. (2012). Lavender essential oil in the treatment of migraine headache: a placebo-controlled clinical trial. *European neurology*, 67(5), 288–291. Link
- Schmerz, C., Koch, C., Mueller, C., et al. (2000). Ibuprofen versus placebo in migraine treatment: a double-blind, randomized, placebo-controlled, dose-ranging study. *Cephalalgia : an international journal of headache*, 20(7), 670–675. Link (*Note: Link abstract differs*)
- Derry, S., Moore, R. A., & McQuay, H. J. (2010). Paracetamol (acetaminophen) with or without an antiemetic for acute migraine headaches in adults. *Cochrane database of systematic reviews*, (11), CD008040. Link (*Note: Link abstract differs*)
- Pascual, J., Mateos, V., Roig, C., Sanchez-del-Rio, M., & Jimenez, D. (2007). Marketed versus generic sumatriptan: a pharmacoepidemiological study. *Headache*, 47(9), 1305–1309. Link (*Note: Link abstract differs*)
- Colman, I., Brown, M. D., Innes, G. D., Grafstein, E., Roberts, T. E., & Rowe, B. H. (2004). Parenteral lorazepam for migraine headaches: a systematic review. *Headache*, 44(4), 369–375. Link (*Note: Link abstract differs*)
- Göbel, H., Fresenius, J., Heinze, A., Dworschak, M., & Soyka, D. (1996). Effectiveness of Oleum menthae piperitae and paracetamol in therapy of headache of the tension type. *Der Nervenarzt*, 67(8), 672–681. Link
- Soković, M., Glamočlija, J., Marin, P. D., et al. (2010). Antibacterial effects of the essential oils of commonly consumed medicinal herbs using an in vitro model. *Molecules*, 15(11), 7532–7546. Link (*Note: Link abstract differs*)
- Seol, G. H., Lee, Y. H., Kang, P., You, J. H., Park, M., & Min, S. S. (2013). Randomized controlled trial for Salvia sclarea or Lavandula angustifolia: differential effects on blood pressure in female patients with urinary incontinence undergoing urodynamic examination. *Journal of alternative and complementary medicine*, 19(7), 664–670. Link (*Note: Link abstract differs*)
- Zargaran, A., Borhani-Haghighi, A., Salehi-Marzijarani, M., et al. (2018). Evaluation of the effect of topical chamomile essential oil on migraine headache: A randomized double-blind placebo-controlled clinical trial. *Complementary therapies in clinical practice*, 31, 1–7. Link (*Note: Link abstract differs*)



Great post! So well researched.
Thank you, Marta! I’ve found the best migraine prevention is to find your personal migraine triggers. I provide in-depth research to help people find and understand the cause of their headaches.
This is such a great post. I suffer from migraines and this is very helpful. I did not know about the migraine pressure points, I will be trying that next time I feel one coming on. Great work on this!!! I will be sharing this with my friends.
Thank you, atripwithaview! Those pressure points help to relieve stress even without a migraine.
Great tips! Thanks for sharing 😌
Thank you, Danielle!!
Very well written and researched. I am bookmarking this page. I have migraine when it’s cloudy, not always though. But this post was super helpful!
Thank you, Suktara29! That is interesting about how you get migraines when it is cloudy. Weather and migraines deserve their own post.
I’ve had migraines since I was a kid, everything here is gold! When I cut out refined sugar, carbs, and processed food in general, the frequency of my migraines exponentially decreased
Thank you, Saila! I’ve learned to appreciate my migraines as they remind me I am doing something unhealthy. Cutting out processed foods also helped me sginificantly reduce my migraines.
These are awesome tips, Jeremy because I know how painful a migraine can be! I’ve suffered through it and for me, lack of sleep, dehydration and hunger and obviously stress are the main triggers. I didn’t think about monitoring my heart rate variability as you mentioned above so I’ll look into as a remedy too but all the other remedies you listed definitely work such as essential oils, massage, yoga, meditation, etc.
Great post!
Thank you, Amira! Yes, monitoring your HRV helps you know when your body is best able to handle stress. Lawyers have a stressful job, I hope these tips help you stay healthy while pursuing your passion.
I get headaches occasionally but that’s usually because of lack of sleep. It’s defutdefin good to be aware of causes and cures for migraines as well.
Thank you, Mary! Yes, sleep is a big one. Migraine causes, triggers and remedies are different for everyone. It is important to learn from multiple people’s experiences.
Great post couldn’t stop myself from sharing
Thank you, Rajesh!
thanks for the list you provided here. This is an awesome blog. More power!
Thank you, Lee!!!
I rarely get migraines. But recently, I’ve discovered that drinking green tea is one of the quickest ways to alleviate a migraine.